Step Into Your Power
Let me show you how to find the power that I know is within you. Sign up for my mailing list and I will send you a free copy of my Five Daily Practices of Self Appreciation.
Treating Heroin and Other Opioid Addiction with Medications

There are different opinions on the subject of recovering from addiction and treating heroin and other opioid dependencies with medications. With the recent death of Philip Seymore Hoffman, the topic of heroin addiction has been getting a lot of attention in the news. In this article I share my opinions about using medications to treat chemical dependency to heroin and other opioids.
What is an “Opioid”
The term “opioid” describes a set of street drugs and medications that are derived from the opium plant – pictured above. The most well known opioid street drug is heroin. Opioid medications are used for the treatment of pain. Examples of well known opioid medications include Morphine, Dilaudid, Vicodin, Percocet, and Oxycontin. Over the past few decades, the abuse of opioid medications has sky-rocketed. In 2008 alone, over 5 million Americans abused pain killers. The field of medicine is beginning to put more and more restrictions on prescribing opioid medications, and this is causing the street price of these medications to go up. As these medications become more and more expensive, people are turning to using heroin which is a cheaper option. We can argue that opioid dependence and addiction is quickly becoming an epidemic in the United States.
What does “Opioid Dependence” Mean
A person develops opioid dependence when he or she cannot stop using opioids. Dependence is both emotional and chemical, meaning that the dependent person struggles with difficult feelings as well as physical withdrawal symptoms when that person tries to stop using the substance. Physical withdrawal symptoms in opioid dependence are extremely uncomfortable and include racing heart, nausea, vomiting, diarrhea, sweating, restlessness, yawning, anxiety, and pain.
Example of Opioid Dependence
Opioid dependence can occur with or without opioid addiction. An example of opioid dependence would be a man who has had several complicated surgeries after a car accident, and who has been on high doses of Vicodin for pain for the past few months. If his pain medications were stopped abruptly, he would most likely go through severe withdrawals. He will need to be weaned off the medications gradually, or go through a detoxification in order to stop his medications. He is chemically dependent on opioids.
Example of Opioid Addiction
Imagine a scenario in which the man in the above example begins to take more Vicodin than was prescribed to him by the doctors. He gets to a point where he wants the pills and craves them whether or not he is in any pain. He begins to run out of the Vicodin, and starts going to different doctors to get more prescriptions. He hides his medication use from his family and feels guilty about it. When doctors refuse to give him more prescriptions, he starts buying Vicodin, Percocet, Oxycontin, and Norco from illegal sources. He tries several times to stop taking the medication, but each time he goes back to using it again. We can safely say that this man is now addicted to the opioids.
Medications Used to Treat Opioid Dependence
Stopping the use of opioids “cold turkey” is really difficult because of the severity of the withdrawal symptoms. Withdrawal symptoms start around twelve hours after the last use of the drug, and are quite severe at twenty four hours after the last use. Many of my patients tell me that they ended up using the drug again because they could not bear the withdrawal symptoms. Even if someone manages to tolerate the initial withdrawals that they experience in the first 1-3 days of not using, they will experience severe muscle and bone pains within about a week after their last use of the drugs.
There are medical choices for stopping the use of opioids. Methadone is one option in which a recovering individual would go to a clinic on a daily basis and get a dose of Methadone. Methadone is itself an opioid medication, and it stops the withdrawal symptoms. People do develop chemical dependency on Methadone, and will have to be weaned off of it gradually. Another newer option is the use of Buprenorphine either by itself (brand name Subutex) or in combination with other medications (brand name Suboxone). Chemical dependency to Buprenorphine also occurs, and people will have to be weaned off of it as well. The reasoning behind using these medications for management of the addiction is that they don’t give the patient the same “high” as the drug does, and therefore have a much lower potential for being abused. Naloxone and Naltrexone are older options that are rarely used any more. Vivitrol is an injection of naltrexone that is newest option in the treatment of opioid addiction. People who take these medications can usually function well and go back to living their daily lives.
A brand new study published in February of 2014 looks at the effectiveness of treatment with Buprenorphine. In this study, data available from different original studies ranging from 1995 until 2012 were analyzed. Based on the data available, it was concluded that treatment of opioid dependence with either Methadone or Buprenorphine show better outcomes than quitting the opioid cold turkey.
Buprenorphine
In my practice, I treat opioid dependence with Buprenorphine. The brand name I mostly use is Suboxone, and I rarely use Subutex. In my experience, Suboxone has been incredibly helpful in the process of helping a person to stop using opioids with very little withdrawal symptoms. This process is very commonly known as “detoxification,” or “detox” for short. I use Suboxone for both the detox process, and sometimes as “maintenance,” depending on my evaluation of each patient.
The detoxification process with Buprenorphine takes anywhere from five to ten days. Consider the case of a woman who has been taking Vicodin for headaches for the past two years, and is now taking about ten to twenty Vicodin pills a day. She would start detoxification by waiting anywhere from twelve to twenty four hours after taking her last Vicodin pill(s). We would wait until she is in “moderate to severe” withdrawal and then give her the first Buprenorphine dose. Usually, relief from withdrawal symptoms comes quickly within five to ten minutes after taking the medication. We would then give her the medication at regular times throughout the next five to ten days, and expect that each day she would have less withdrawal symptoms. After the detoxification phase is over, we would talk about maintenance.
Advantages of using Buprenorphine are numerous. Patients usually can tolerate the medication well, and they manage to stop their use of opioids with much less difficulty than trying to stop cold-turkey. In the addiction world, opioid withdrawal is so severe that the process of using more opioids to stop the withdrawal symptoms is referred to as “getting well.” I find it very ironic that the process of drug use is known as getting well, since there is nothing healthy about abusing opioids. Buprenorphine can keep away most of the withdrawal symptoms, without giving the individual a “high” that normally comes with abusing opioids. Although many rehabilitation facilities have adopted the use of Buprenorphine in the detox process, there is still a lot of resistance to using Buprenorphine as a means to maintain sobriety. There is a belief that one is not truly sober while they are using Buprenorphine. One of the reasons behind this belief is the fact that Buprenorphine itself has withdrawal symptoms when patients decide to stop taking the medication.
I prefer work with each patient individually to understand what his or her needs are rather than making a blanket statement about what sobriety means. For example, for a patient that has had a short term dependence on opioids, is trying to quit it for the first time, and does not have other complicating factors, I usually suggest using Buprenorphine for managing the withdrawal symptoms, and slowly wean him or her off of the medication. On the other hand, if I have a patient who has been using a lot of opioids over a long period of time, has tried several times to quit the drugs and has relapsed every time, has resorted to injecting the drugs intravenously (IV), and most importantly, if he or she has a history of overdosing on the drug, then I discuss use of Buprenorphine as a maintenance tool. Either way, it is important to talk to each person individually and try to come up with a treatment plan that works for him or her. Generalizations are usually not a good idea when it comes to such a life-threatening disease.
Buprenorphine use has its disadvantages as well. When a patient is on Buprenorphine, he or she cannot get a high from using opioid drugs. Some people keep using more and more drugs to get the high, and end up overdosing. Another disadvantage of using Buprenorphine is that come patients just plan their relapses ahead of time, and stop taking Buprenorphine a day or two before their planned relapse.
The disadvantages listed above are cause for serious concern, and are the reason why Buprenorphine treatment should be closely monitored by an experienced physician. Patients that relapse and continue using opioids while on Buprenorphine are probably not good candidates for the medication. I don’t see any point in prescribing Buprenorphine for someone who is not yet committed to becoming sober.
Methadone
The process of detoxification using Methadone is similar to the process of using Buprenorphine. The person stops using their drug, and when in withdrawal, begins taking Methadone as prescribed by his or her physician.
Methadone maintenance has been around for a while, and it has been known to have positive outcomes. Methadone maintenance has the same disadvantage as Buprenorphine in that people can just plan their relapses by not taking the medication. Additionally, being on Methadone maintenance requires the person in treatment to go to a clinic on a daily basis. Some also argue that the use of Methadone itself gives the user a high, and therefore is not compatible with sobriety. I believe that using either Buprenorphine or Methadone for maintenance of sobriety is acceptable. In my practice, I use Buprenorphine.
Vivitrol
A relatively newer alternative to Methadone and Buprenorphine comes in the form of Vivitrol (Naltrexone) injections. This is a shot that is given once a month. Vivitrol has been shown to prevent the symptoms of craving, and to prevent the individual from getting a high if he or she uses opioids while on Vivitrol. There is a risk of overdosing on opioid drugs while on Vivitrol as well as Buprenorphine, and there are less studies available for it. My patients, however, like the convenience of once a month injections. They also like the fact that once injected, the medication stays in their bodies for a month, and they cannot choose to skip a dose as easily as they can with Suboxone.
Summary
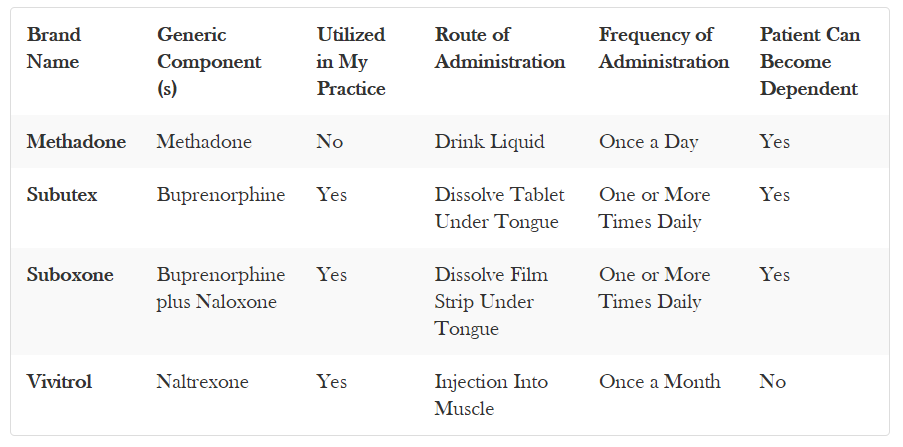
This table summarizes the medications discussed above.
Conclusions
Studies from 1995 until recently have pointed out the benefits of using medications to manage opioid addiction. Medications have been shown to be useful in both detoxification off of the drugs, and maintenance of sobriety. Although benefits of these medications have been shown, they are definitely not for everyone. They are also not enough by themselves. People who are most dedicated to their sobriety will “work a program” on a daily basis. Addiction is a complicated disease with a heavy psychological component. Although medications can be helpful in management of opioid addiction, achieving and maintaining sobriety requires life-long dedication and hard work.
Doctor Life Advice
